Healthcare leaders in the UK — from NHS trust managers to CIOs and finance directors — face the same pressure: deliver faster claims processing with fewer resources, while staying compliant with strict regulations. Manual claims handling, paper-based forms, and disconnected systems consume staff time and slow reimbursements, diverting attention away from patient care.
That’s why many UK providers are investing in healthcare claims management software. The right system digitises approvals, reduces errors, and provides executives with visibility into every claim.
It also supports the government-mandated drive to improve NHS productivity, helping providers save millions while directing more effort toward patient outcomes
In this guide, we’ll compare the top healthcare claims management systems software in 2026 and show why FlowForma is the most cost-effective, transparent, and adoption-friendly choice for providers seeking measurable ROI.
What Is Healthcare Claims Management?
 What is healthcare claims management?
What is healthcare claims management?
Healthcare claims management refers to the process of handling medical and insurance claims from submission through adjudication to payment. Healthcare claims management software automates these workflows, reducing manual effort, minimising errors, and improving efficiency.
By supporting the entire claims lifecycle — including claims submission, validation, processing, and reporting — these systems help healthcare organisations ensure accuracy, compliance, and timely reimbursement. AI-driven tools can further enhance the process, enabling faster claim approvals and better data-driven decisions.
Using healthcare claims management software helps reduce administrative costs, streamline operations, and improve communication between healthcare providers, insurers, and patients.
Key Features of Claims Management Software
 Key features of claims management software
Key features of claims management software
Healthcare claims management software typically includes features that enhance efficiency, accuracy, and security:
- Claims Data Capture: Collects and securely stores patient documentation, medical records, and claim-related information.
- Automated Workflows: Streamlines approval, submission, and processing steps to reduce manual tasks and accelerate turnaround times.
- Document Management: Centralised storage and easy retrieval of claim files for faster processing.
- Fraud Detection & Validation: Flags inconsistencies or errors to prevent denied claims and ensure compliance.
- Real-Time Analytics: Provides visibility into claim status, bottlenecks, and performance metrics for better decision-making.
10 Best Healthcare Claims Management Software in 2026
Here’s a quick overview of the top 10 healthcare claims management software UK for 2026:
|
Software
|
Best For
|
Integrations
|
No-code
|
|
FlowForma
|
Mid-to-large healthcare providers seeking transparent pricing, fast adoption, and compliance-ready claims workflows
|
Microsoft 365, SharePoint, and other systems
|
Yes
|
|
CMW Lab
|
Healthcare project and claims workflows with a strong collaboration focus
|
Microsoft 365, Salesforce, Google Workspace
|
Partial
|
|
ModMed
|
Private practices needing specialty-specific claims support
|
EHRs, lab systems, and billing tools
|
No
|
|
athenahealth
|
Mid-to-large practices seeking payer connectivity and revenue cycle management
|
300+ payers, EHR integrations
|
Limited
|
|
Inovalon
|
Data-driven claims processing for payers and providers
|
Proprietary healthcare data cloud
|
No
|
|
Pegasystems
|
Complex healthcare claims at enterprise scale
|
Legacy systems, CRM, ERP
|
Limited
|
|
Kissflow
|
SMEs needing simple process digitisation across industries
|
Microsoft 365, Google Workspace
|
Yes
|
|
RXNT
|
Small to mid-size practices focused on billing and e-prescribing
|
Pharmacy systems, billing clearinghouses
|
No
|
|
MindBowser
|
Custom-built claims automation and healthcare apps
|
API-driven, bespoke system connections
|
No
|
|
DrChrono
|
Practices needing EHR + billing integration in one platform
|
iPad/iOS apps, labs, billing systems
|
Limited
|
10 Top Healthcare Claims Management Software in 2026
Now, let us break down the 10 medical claims software and analyse their key features, pros, and cons.
1. FlowForma
FlowForma stands out as a top healthcare claims processing software
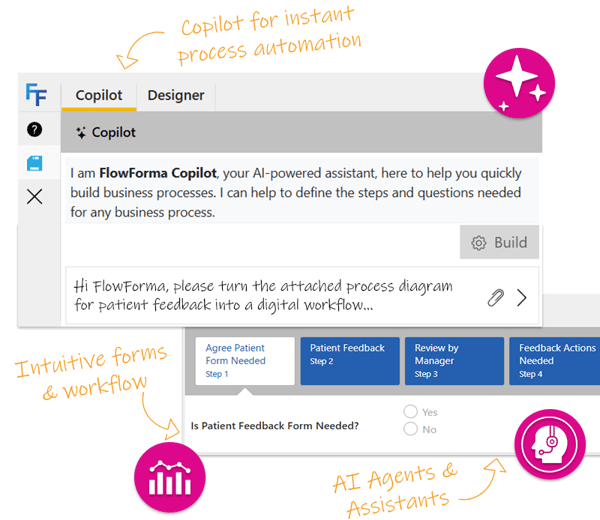
FlowForma is an AI-powered business process automation tool designed to simplify and automate medical claims management. Widely adopted across NHS hospitals (such as Blackpool NHS) and private providers, it helps healthcare organisations eliminate manual paperwork, digitise approval workflows, and maintain compliance with audit trails.
What makes FlowForma distinct in the healthcare claims management software market is its transparent pricing and absence of hidden costs. Additionally, it is a listed vendor on the G-Cloud 13 Framework, Microsoft 365, and the NHS London Procurement Partnership.
Also read: A complete guide to healthcare claims automation
FlowForma Key Features
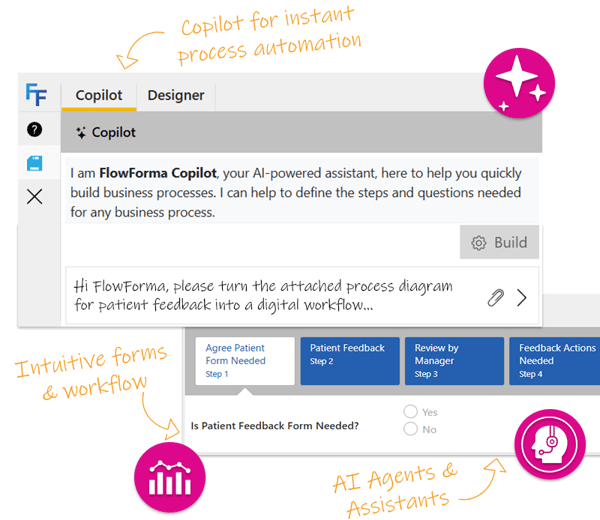
With a no-code platform and powerful AI-driven automation, FlowForma helps healthcare organisations improve efficiency, reduce errors, and ensure compliance, all while accelerating the entire claims management process.
1. No-code automation of claims workflows
In healthcare, claims workflows can involve multiple stages and stakeholders: from eligibility verification, coding, and claims submission to follow-ups and resubmissions.
FlowForma allows healthcare administrators to design these workflows using an intuitive user interface, ensuring that multiple departments — from finance to compliance — can participate in a streamlined, automated process.
Watch this demo to see how FlowForma automates a medical claims processing workflow.
2. Automated document generation
FlowForma automates the creation of claims submissions, audit reports, and compliance certificates. With data pulled directly from the workflow, the tool populates pre-built templates with the most current information, ensuring that documents are always accurate, up-to-date, and auditable.

Automate creation of claims documents using FlowForma
By automating document generation, healthcare organisations reduce administrative workloads, improve data accuracy, and avoid compliance risks, ultimately speeding up the claims cycle and reducing operational costs.
3. AI suite for intelligent claims management
FlowForma’s AI Suite brings intelligent automation to healthcare claims management. Key features within the suite include:
- AI Copilot: Enables users to create complex claims workflows simply by describing them in natural language. The AI instantly builds the workflow, with the necessary steps and logic, while ensuring compliance with GDPR, HIPAA, and NHS legistlation .

Automate claims management process using FlowForma’s AI Copilot
- AI Agents: AI Agents automate the validation of claims and ensure data accuracy by cross-checking submitted claims against regulatory standards. It can also extract structured data from unstructured documents, reducing manual entry and speeding up the process.
- AI Summarisation: Provides access to real-time, concise summaries of workflow steps. This enhances transparency, enabling stakeholders to make faster and more informed decisions
- Smart Assistants: Allows users to interact with claims workflows via natural language commands, such as “Submit claim” or “Validate patient data.” This eliminates the need for training, allowing anyone to quickly engage with complex processes.
- Ambient Discovery Agent: Analyses claim documentation and workflows to identify automation opportunities, helping providers detect bottlenecks and streamline processing.
FlowForma’s discovery agent
4. Audit trails and regulatory compliance
Healthcare claims processing requires strict compliance with regulations like the Data Protection Act 2018 and GDPR, as well as NHS guidelines.
FlowForma’s in-built compliance module ensures that every step in the claims process is auditable, from initial submission to final approval. These built-in features generate audit trails that track all user interactions, modifications, and approvals, providing a transparent and verifiable record for compliance and reporting purposes.
5. Seamless integrations
FlowForma integrates seamlessly with Microsoft 365, SharePoint, Teams, and over 1,000 other systems. Whether you're managing claims, tracking patient data, or coordinating between departments, FlowForma ensures all systems work together efficiently.
FlowForma Pros
- Listed vendor on the G-Cloud 13 Framework, N365 and NHS London Procurement Partnership
- Transparent pricing structure with no hidden costs, reducing the total cost of ownership
- Form and document management features for effective claims management
- Rapid adoption rates due to intuitive no-code design and Microsoft 365 familiarity
- AI Copilot, Agentic AI and other AI features for intelligent and context-aware claims management automation
FlowForma Cons
- Requires a Microsoft 365/SharePoint environment, which may be restrictive for organisations outside that ecosystem
FlowForma Pricing
FlowForma offers tiered, transparent pricing with no hidden costs. Pricing is based on the number of processes automated, allowing organisations to scale their automation efforts predictably.
This predictability is crucial for mid-sized and large healthcare organisations aiming to establish an effective automation program.
Also read - Automation in healthcare: benefits and examples in 2026
💡Case Study in Focus: How Blackpool Teaching Hospitals NHS Streamlined Healthcare Processes

Blackpool Teaching Hospitals NHS Case Study
Blackpool Teaching Hospitals NHS faced significant challenges managing complex hospital workflows, including claims, staff approvals, and compliance reporting. Manual paper-based processes caused delays, errors, and frustration among staff, while siloed systems made it difficult to track progress across departments.
FlowForma’s no-code process automation platform was deployed to digitise and streamline hospital workflows. Dynamic forms replaced paper processes, while AI-powered features automated approvals and claims validation. Integrated audit trails and compliance reporting ensured all actions were transparent and aligned with NHS regulatory standards.
|
“A process automation solution that can be procured easily for NHS Trusts like ours is key to assisting wider transformation across the entire NHS ecosystem. We hope we can act as a successful business case for others to follow in the future.”
- Mark Greenwood, Senior Developer at BTH
|
2. CMW Lab
 CMW Lab home page
CMW Lab home page
CMW (Comindware) Lab is a process and project management tool with healthcare claims workflow capabilities. It focuses on collaboration and transparency across complex processes, making it suitable for NHS teams seeking clear communication across departments.
CMW Lab Key Features
- Visual workflow designer for claims handling
- Cross-department collaboration dashboards
- Prebuilt templates for healthcare processes
- API-based integration with EHR and billing systems
- Role-based permissions for compliance and data security
CMW Lab Pros
- Strong collaboration features with visibility across teams
- Flexible customisation of claims workflows
- Cloud and on-premise deployment options
- Secure role-based access suitable for regulated industries
CMW Lab Cons
- Steeper learning curve compared to no-code competitors
- Limited AI-powered automation features
3. ModMed
 ModMed homepage
ModMed homepage
ModMed is a healthcare-specific platform widely used in private practices. It combines EHR, practice management, and claims processing in one integrated tool, tailored to specialty needs such as dermatology, orthopaedics, and ophthalmology.
ModMed Key Features
- Specialty-specific coding assistance for claims
- Integrated practice management and billing modules
- Real-time eligibility and claims scrubbing
- Reporting and analytics for reimbursement trends
- Mobile-friendly platform with iPad apps
ModMed Pros
- Deep specialty-specific functionality
- Integrated billing and clinical workflows
- Real-time claims validation reduces denials
- Strong user adoption in the US private practice market
ModMed Cons
- Less suited for NHS-scale workflows
- Pricing can be prohibitive for smaller practices in the UK
4. athenahealth
 athenahealth homepage
athenahealth homepage
athenahealth offers revenue cycle management and claims automation with extensive payer connectivity. Known for its cloud-based network, it streamlines claims submission and follow-up across hundreds of insurers.
athenahealth Key Features
- Cloud-based claims submission to 300+ payers
- Built-in claims scrubbing and eligibility checks
- Integrated scheduling, billing, and reporting
- Patient portal with payment tracking
- Analytics dashboards for reimbursement insights
athenahealth Pros
- Wide payer connectivity
- Strong revenue cycle management focus
- User-friendly interface for billing teams
- Integrated scheduling and patient communication tools
athenahealth Cons
- High cost for UK adoption outside its US stronghold
- Limited customisation for NHS-specific workflows
5. Inovalon
 Inovalon claims management page
Inovalon claims management page
Inovalon is a data-focused healthcare claims management system, widely used by payers and large providers. It excels in analytics, risk adjustment, and compliance.
Inovalon Key Features
- Proprietary healthcare data cloud for insights
- Claims validation and adjudication automation
- Risk adjustment and predictive modelling
- Integration with payer systems
- Compliance-focused audit trails
Inovalon Pros
- Strong data analytics and reporting capabilities
- Proven adoption among payers and insurers
- Advanced compliance and risk adjustment support
- Scalable for enterprise-level organisations
Inovalon Cons
- Complex implementation process
- Less suitable for smaller NHS trusts or clinics
6. Pega
 Pega’s claims management page
Pega’s claims management page
Pega is an enterprise-grade process automation tool, widely adopted in financial services and healthcare. It supports highly complex claims workflows for large organisations.
Pegasystems Key Features
- Advanced business rules engine for claims adjudication
- Case management for complex healthcare claims
- Integration with legacy systems and CRMs
- AI-driven decisioning for claims validation
- Enterprise-grade compliance and audit trails
Pegasystems Pros
- Highly customisable enterprise automation
- Robust AI decisioning capabilities
- Proven track record in large-scale deployments
- Strong compliance and audit support
Pegasystems Cons
- Requires significant IT resources to implement
- High cost compared to no-code competitors
7. Kissflow
Kissflow’s healthcare solutions page
Kissflow is a no-code platform for process automation across industries. It includes claims management templates but is more generic compared to healthcare-specific competitors.
Kissflow Key Features
- Drag-and-drop process builder
- Prebuilt claims workflow templates
- Integration with Microsoft 365 and Google Workspace
- Reporting and analytics dashboards
- Cloud-native, mobile-ready design
Kissflow Pros
- Simple and intuitive no-code builder
- Affordable for SMEs
- Good for quick wins in digitisation
- Wide integration options
Kissflow Cons
- Limited healthcare-specific functionality
- Less suitable for NHS-scale complexity
8. RXNT
RXNT homepage
RXNT is an EHR and practice management solution popular among small and mid-size practices. It includes claims processing features integrated with billing and prescribing.
RXNT Key Features
- Integrated billing and claims submission
- Real-time eligibility checks
- e-Prescribing and scheduling
- Patient payment tracking
- Cloud-based mobile access
RXNT Pros
- Affordable for smaller practices
- Integrated claims and billing functionality
- Easy-to-use interface
RXNT Cons
- Limited adoption in the UK healthcare sector
- Not built for NHS-scale workflows
9. MindBowser
 MindBowser homepage
MindBowser homepage
MindBowser offers custom-built claims management systems, designed for providers needing tailored automation. It is less an off-the-shelf solution and more a development partner.
MindBowser Key Features
- Custom claims automation software
- API-based integrations
- Data-driven reporting tools
- Security and compliance features
- Bespoke development services
MindBowser Pros
- Tailored solutions to exact client needs
- Flexible integration capabilities
- High level of customisation
- Dedicated development support
MindBowser Cons
- Longer implementation timelines
- Higher upfront costs compared to SaaS tools
10. DrChrono
DrChrono’s homepage
DrChrono is a cloud-based EHR and billing platform with integrated claims processing. It is best suited for practices looking for a combined clinical and financial tool.
DrChrono Key Features
- EHR and claims billing in one platform
- Real-time eligibility verification
- Patient portal with claims visibility
- Reporting dashboards
DrChrono Pros
- Integrated clinical and claims workflows
- Mobile-friendly for clinicians on the go
- Real-time claims validation
- User-friendly design
DrChrono Cons
- Limited scalability for NHS-sized deployments
- Focused mainly on the US private practice market
Why FlowForma is the best medical claims management software
Hear from Blackpool Teaching Hospitals NHS on the benefits of FlowForma Process Automation
Healthcare claims management software is no longer optional for NHS trusts and UK providers seeking to reduce administrative costs, improve accuracy, and accelerate reimbursements. While many global tools exist, not all fit the compliance-heavy, resource-constrained environment of UK healthcare.
FlowForma stands out as the best healthcare claims management software for NHS and UK providers, thanks to:
- Transparent pricing with no hidden costs
- Proven adoption within NHS hospitals and trusts
- Rapid ROI within weeks, not months
- AI-powered automation via FlowForma Copilot and Agents
- Seamless integration with Microsoft 365 and existing systems
👉 Book a demo today to see how FlowForma can accelerate claims management in your healthcare organisation.
.png)