Manual claims management can drain resources and slow growth. Paper-heavy workflows delay settlements, errors trigger costly rework, and fraud inflates loss ratios.
Adjusters waste valuable hours on repetitive tasks instead of focusing on high-value cases, while compliance teams face blind spots across different jurisdictions. The result: higher costs, lower productivity, and dissatisfied customers.
AI changes this equation. By automating routine processes, accelerating reviews, and flagging risks in real-time, it enables insurers to process more claims without adding headcount. The outcome is clear: lower operating costs, reduced leakage, faster settlements, and improved customer retention.
Below are 10 ways AI is reshaping claims management and delivering measurable returns for insurers today.
How AI Helps Claims Now and In The Future
AI is transforming claims processing, from intake to settlement. A Coleman Parkes study of 236 insurance decision-makers found that 9 out of 10 plan to invest in generative AI within the following year.
While insurers highlight data privacy, security, training, governance and transparency as key concerns, AI is already streamlining manual tasks, reducing errors and improving fraud detection—delivering faster, more accurate outcomes for insurers and policyholders.
Let’s briefly walk through the current use cases of AI in claims processing, as well as how it is envisioned in the future:
AI in claims processing today
 How is AI used in claims processing now?
How is AI used in claims processing now?
AI is already delivering measurable returns across the claims lifecycle by reducing loss costs, cutting administrative overhead, and speeding up settlements:
- First Notice of Loss (FNOL): Telematics, IoT sensors, and chatbots capture data at the source, reducing manual entry and ensuring faster and cleaner claim intake.
- Investigation and coverage: OCR eliminates paperwork backlogs, while computer vision and drones cut inspection times from days to hours—improving accuracy and lowering field costs.
- Valuation and payments: Predictive analytics generate real-time estimates, while automated payment tools release approved funds instantly, improving cash flow for policyholders and reducing cycle times for insurers.
- Fraud detection: Machine learning detects duplicate claims, inflated costs, and staged accidents early, protecting margins and ensuring genuine claims are paid promptly.
- Compliance and reporting: Automated audit trails reduce the burden on compliance teams, lower the risk of fines, and maintain records that are regulator-ready across jurisdictions.
- Customer communication: Virtual assistants provide proactive status updates, reducing inbound calls and boosting customer satisfaction—leading to higher retention.
- Analytics and forecasting: AI monitors claim volumes, identifies bottlenecks, and predicts workloads, enabling insurers to scale operations without proportional increases in headcount.
AI in claims processing in the future

Emerging AI applications in claims processing
Emerging applications promise even greater efficiency, risk control, and competitive differentiation:
- Generative AI: Automates end-to-end workflows from uploaded forms or natural language prompts, cutting process design costs and reducing dependency on IT.
- Autonomous agents: Fraud checkers, assessors, and approval agents can operate in parallel, compressing multi-step claims into near real-time settlements.
- Predictive risk modelling: Anticipates claims before they occur—such as weather-driven property damage—helping insurers price risk accurately and reduce exposure.
How are Insurers Using AI for Claims Processing?
 How insurers are using AI for claims processing and management
How insurers are using AI for claims processing and management
Insurers are adopting artificial intelligence to streamline and expedite claims. AI-based solutions improve efficiency, lower costs and make claims more accurate. It also helps claims professionals detect fraud, improve customer service and prepare for future risks.
1. Automating claims handling
AI extracts data from forms, bills, reports and photos, reducing manual errors and delays. With FlowForma’s AI Agent Rule, insurers can automate intelligent actions that traditionally caused delays and errors. Acting as an AI-powered assistant, it reads uploaded documents, extracts structured data, validates and formats content and seamlessly returns results to forms or systems.
For example, it can process forms, bills, reports and even photos, reducing manual effort while improving accuracy.
In addition, insurers can also go a step further with FlowForma’s AI Copilot. Claims teams can create an end-to-end handling process in minutes by simply uploading existing forms or describing the workflow in plain language. Watch this demo on healthcare claims process to learn more.
 Create seamless claims process using FlowForma’s AI Copilot
Create seamless claims process using FlowForma’s AI Copilot
In this example above, you'll see a detailed prompt from the user listing all the requirements needed within the process.
Following the prompt, FlowForma Copilot automatically builds a structured workflow with forms and steps in the process.
 Insurance claims form generated by FlowForma Copilot
Insurance claims form generated by FlowForma Copilot
To help you visualise the process steps, FlowForma Copilot also creates a structured process map as shown below.

Process map created by FlowForma Copilot
You can continue to refine your process, use suggested enhancements, and ask FlowForma Copilot for recommendations to complete the match the claims process to your specfic business requirements.

FlowForma Copilot chat feature to add steps and rules
This enables faster claims setup, consistent execution and easier compliance, while giving staff more time to focus on complex cases that require human intervention.
Want to test FlowForma Copilot out for yourself? See how fast, simple, and intuitive it is to automate insurance claims in the FlowForma Playground.
2. Enhancing fraud detection for complex claims
AI models scan claims for unusual patterns, duplicate submissions and inflated costs. By cross-checking details against historical and external data, they flag suspicious cases early. This reduces losses while ensuring genuine claims are paid quickly.
FlowForma strengthens this stage with Agentic AI. Its tools extract and validate information, generate clear summaries for adjusters and route claims intelligently based on complexity or risk—as shown in the image below.
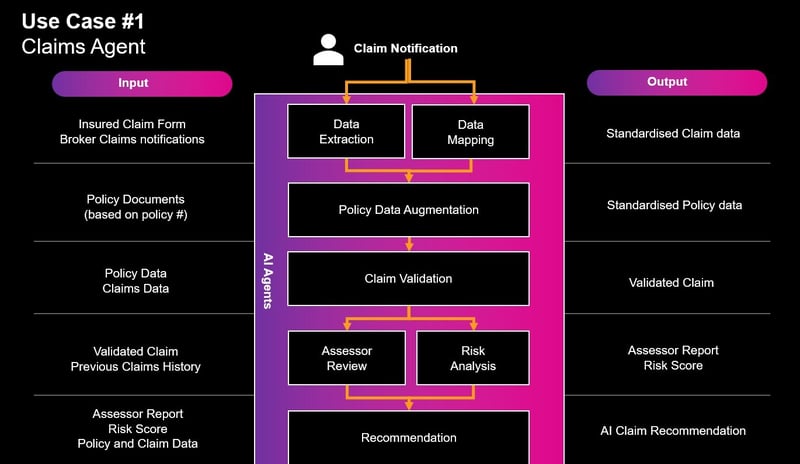
AI claims agent
Learn more about FlowForma's claim agent in this video:
For instance, Agentic AI can scan a police report, capture key details such as time, location, incident type, etc., and automatically populate them into the claim file.
It can then create a concise case summary highlighting issues that need attention, allowing adjusters to focus on decisions instead of manual review.
3. Improving customer and claims experience
Virtual assistants and chatbots guide policyholders through the claim submission process. They answer common questions and provide real-time status updates. These tools also support staff with quick access to information, reducing delays and improving communication. It’s no surprise, then, that insurers see this as a top priority.
A 2024 survey, The Carrier Perspective: 2024 Claims Insights, found that 67% of insurers are already using AI in customer service and 45% in claims handling.
4. Streamlining risk management for better outcomes
Predictive models forecast claim volumes, costs and reserves, helping insurers focus on high-risk cases and allocate resources effectively. They also generate audit trails to support compliance.
Using FlowForma’s no-code process automation platform, claims teams can set custom rules, connect to real-time data sources and generate dynamic risk scores for each claim.
For instance, a claim involving multiple parties and high estimated costs can be automatically flagged as high risk, routed to senior adjusters, and tracked closely with complete visibility.
This accelerates risk analysis, reduces bottlenecks and ensures compliance is built into every stage of the process.
5. Automating document generation
With FlowForma’s document generation feature, tasks are built directly into the claims process.
For example, once a claim is approved, the system can automatically generate a settlement letter with the claimant’s details, policy information and payment amount pre-filled. If additional evidence is required, the workflow can produce a tailored request letter with the correct formatting and branding.
Audit-ready reports are automatically generated at every claims stage, ensuring compliance with minimal manual effort. This cuts drafting work, improves accuracy and speeds communication with policyholders and regulators.
What are the Benefits Offered by AI in Claims Processing?
 5 benefits of AI in claims processing
5 benefits of AI in claims processing
AI delivers measurable improvements for insurers and policyholders alike, helping reduce costs, strengthen controls, and improve customer outcomes.
With no-code platforms like FlowForma, insurers can combine automation and AI to accelerate claims management while ensuring governance and compliance.
1. Faster and more accurate claims handling
Automated intake, document validation, and data extraction reduce manual errors and shorten settlement times. With FlowForma, insurers can instantly design and deploy claims workflows, handling higher volumes without delays.
Here’s a quick demo of FlowForma AI Copilot creating a claims handling process in just a few steps:
2. Improved fraud detection and risk management
AI models flag suspicious activity early, cutting fraud-related losses and protecting margins. FlowForma’s AI Copilot enables insurers to define structured risk rules, automate data collection, and carry out real-time risk assessments.
3. Cost savings and scalability
By removing manual effort, AI lowers administrative costs and eliminates rework. With tools like FlowForma, users can scale without proportional increases in staff or expense.
Essentially, the platform’s transparent, all-in pricing model also makes financial planning predictable, avoiding the hidden fees.
4. Enhanced and seamless customer experience
Faster decisions, instant updates and self-service portals create a transparent process that strengthens policyholder trust. FlowForma’s automation ensures more transparent communication and speedier implementation—up to 10x faster than traditional approaches.
Find out why leading Insurer Aon chose FlowForma in this video:
5. Data-driven insights
AI-powered analytics provide real-time visibility into claim volumes, risks and resource needs. FlowForma adds governance and auditability, enabling leaders to make confident, data-backed decisions.
6. Compliance and governance
Automated audit trails, document generation, and standardised workflows reduce regulatory risk and provide compliance teams with the visibility they need across jurisdictions.
Real-World Examples of AI in Claims Processing: How Aon Transformed Compliance and Efficiency
As part of its digital transformation strategy, Aon, one of the largest insurance brokers in Ireland, wanted to streamline operations, reduce manual effort and strengthen compliance.
The challenges
The company faced inefficiencies caused by different business units running processes their own way, often using Excel, email and paperwork. In addition, SharePoint workflows were too clunky, lacked visibility and provided no audit trail.
This created compliance risks and slowed down critical activities such as HR onboarding, GDPR requests, internal transfers and insurance vetting. The business needed a centralised, automated system that could support compliance, improve efficiency and drive adoption across teams.
The solution
Aon implemented FlowForma Process Automation to digitise and standardise workflows within Microsoft.
Using FlowForma’s no-code platform, the IT team and business users quickly built processes for HR onboarding/offboarding, GDPR compliance, insurance vetting, complaints and IT outages.
The Design Manager allowed creation in days, with no complex training, while providing a central repository, audit trails and intuitive functionality that encouraged adoption beyond IT.
Dive deep into Aon’s successful implementation of FlowForma
The outcomes
FlowForma cut process build times from months to days, improved compliance and boosted efficiency. The Insurance Vetting System, previously reliant on paperwork, evolved into a real-time workflow that now takes minutes.
More business units adopted FlowForma, with non-IT staff building processes independently. The IT team can now scale automation, supporting Aon’s digital transformation while managing repetitive tasks faster, easier and transparent.
 Robbie Molloy’s feedback on FlowForma implementation
Robbie Molloy’s feedback on FlowForma implementation
Streamline Claims Automation with FlowForma’s AI Innovations
Hear why leading insurers choose FlowForma
FlowForma combines no-code automation and AI to simplify claims management, reduce costs, and improve compliance. Insurers can deploy workflows in hours, scale without adding headcount, and deliver faster, more transparent service to policyholders.
Key features include:
- AI Copilot: Instantly builds claims workflows from uploaded forms or natural language descriptions, removing manual setup and accelerating implementation.
- Agentic AI: Extracts and validates claim data, summarises documents and routes cases intelligently across the claims journey from FNOL to settlement.
- Discovery Agent: Converts conversations, calls, or documentation into ready-to-use processes, helping insurers capture requirements without writing prompts.
- Automated document generation: Creates settlement letters, compliance reports and approval notices automatically, cutting administrative effort and reducing errors.
- Audit trails and governance: Every claim is logged with full accountability, ensuring consistent compliance and reducing regulatory risk.
- Seamless integration: Works natively with Microsoft 365 and connects with 1,000+ external systems for smooth adoption without IT disruption.
With FlowForma, claims professionals can accelerate claims processing, improve compliance and deliver superior customer experiences—fast.
Start a 7-day free trial today to see FlowForma in action.
.png)












![Reinsurance Claims Management 101: All You Must Know [2026]](https://www.flowforma.com/hubfs/Claims-management-in-reinsurance.webp)


